VOLUME 33, ISSUE 2
Alexander Reskallah, M.D.
Assistant Professor
Department of Anesthesiology
UT Health McGovern Medical School
Houston, TX

Sara Guzman-Reyes, M.D.
Associate Professor
Department of Anesthesiology
UT Health McGovern Medical School
Houston, TX

Johanna B. De Hann, M.D.
Assistant Professor
Department of Anesthesiology
UT Health McGovern Medical School
Houston, TX

Srinath Sridhar, M.D.
Associate Professor
Department of Anesthesiology
UT Health McGovern Medical School
Houston, TX

Evan G. Pivalizza, MBCHB, FASA
Professor
Department of Anesthesiology
UT Health McGovern Medical School
Houston, TX
What Anesthesiologists Should Know About Kidney Transplantation in Texas in 2021
Donation Trends, Data
Texas mirrors continued positive national trends in organ donation and kidney transplants (KTs) with 2,163 completed in our state in 2020 (1,550 deceased donor [DD], 613 living donor respectively) (https://optn.transplant.hrsa.gov/data/view-data-reports/state-data/#). Texas is served by 3 geographic organ procurement organizations (Figure 1), all are founding members of the Donate Life Texas organ, eye and tissue donor registry (https://www.donatelifetexas.org/). There are 26 active kidney transplant centers of varying size (Figure 2) whose individual activity, speed of recipient access to a DD kidney and 1 year kidney survival data compared to national rates, is accessible via the Scientific Registry of Transplant Recipients (SRTR) (https://www.srtr.org/transplant-centers). Enthusiasm remains tempered by the sobering 9746 patients currently on the kidney waiting list and the continued attrition due to death on the waitlist (484 in 2020) and those who became too ill for transplant (588 in 2020).
Outstanding results for both patient (> 97%) and graft (> 95%) 1-year survival support KT as the definitive therapy of choice for patients with end-stage kidney disease (ESRD) with 5 year graft survival remaining 80 % (SRTR annual report, https://onlinelibrary.wiley.com/doi/epdf/10.1111/ajt.16502).
Kidney Allocation System
Given concerns of potential disparity in allocation of DD kidneys, the Organ Procurement and Transplantation Network (OPTN) introduced a new kidney allocation system (KAS) in 2014 with subsequent improvements in equitable access and reduced wait times for highly sensitized recipients with more challenging cross-matching. The allocation system evaluates:
- Quality of the donor kidney (Kidney donor profile index (KDPI)), scored from 0% – 100% based on 10 donor factors (a lower number predicts better graft survival),
- Anticipated survival of recipient (Estimated post-transplant survival (EPTS)) where older age, longer dialysis duration, prior organ transplant, and diabetes led to a higher score, or worse predicted graft survival,
- Optimal matching is a top 20th EPTS % (better predicted survival) with a kidney with lower risk of graft failure (KDPI < 20%) risk of graft failure).
Additional modifications to organ allocation are based on a 250-nautical mile fixed radius around the donor hospital with a formula for proximity points inside and outside the circle, increased priority for prior living donors, pediatric candidates, and an added medically urgent category.
Post-KAS implementation data confirm increased transplants in patients with >5 years dialysis as well as African-American recipients. Also noted was wider geographic organ sharing, especially for higher KDPI kidneys and this has led to a slight increase in discard rates, cold ischemic times (CIT) and delayed graft function (DGF) which have not adversely impacted continued excellent outcomes. This is partly related to the routine use and positive impact of hypothermic machine perfusion of donated kidneys.
Anesthetic Implications
Consideration of longer dialysis burdens for recipients and the increased CIT and DGF are relevant for anesthesiologists who may face challenging vascular access in the former and delayed diuresis and kaluiresis at the end of the procedure (1).
Enhanced recovery after surgery (ERAS) protocols are appropriate for KT recipients, apart from avoiding non-steroidal anti-inflammatory drugs. Additionally, the lower quadrant incision is favorable to truncal regional analgesic techniques: we perform lateral or posterior quadratus lumborum blocks for all KT recipients with favorable preliminary opioid-sparing results (2). Recent expert recommendations for perioperative fluid management (3) include:
- Low quality evidence for larger volume fluid administration targeting higher central venous pressure (CVP), although targeted acceleration of fluid administration immediately prior to reperfusion may be useful,
- Use of CVP as a guide for fluid administration is only weakly supported,
- Reports of dynamic indices of volume status are promising, but limited,
- Balanced crystalloid solutions offer a better metabolic profile and equal, if not lower, serum potassium levels compared to 0.9 % saline and are strongly recommended.
Conclusion
Despite positive trends in KT rates, equitable organ access, and surgical outcomes, the dire need for donated organs (deceased and living) remains. ESRD patients, especially those on dialysis, should be offered an opportunity for transplant evaluation. KT recipients may present greater management challenges to anesthesiologists. Prospective data is necessary to support promising developments in regional anesthesia techniques, ERAS protocols, and objective fluid management.
References
- Sridhar S, Guzman-Reyes S, Gumbert SD et al. The New Kidney Donor Allocation System and Implications for Anesthesiologists. Semin Cardiothorac Vasc Anesth. 2018: 22; 223-8. doi: 10.1177/1089253217728128
- de Haan JB, Balogh JG, Clendeninn DJ, et al. Quadratus Lumborum Block for Renal Transplant Recipients. Anesthesiology A2058, 2018 (abstract)
- Wagener G, Bezinover D, Wang C et al. Fluid Management during Kidney Transplantation: Consensus Statement of the Committee on Transplant Anesthesia of the ASA. Transplantation. 2020 Dec 14. doi: 10.1097/TP.0000000000003581
Figure 1. Geographic coverage of the 3 Organ Procurement Organizations in Texas
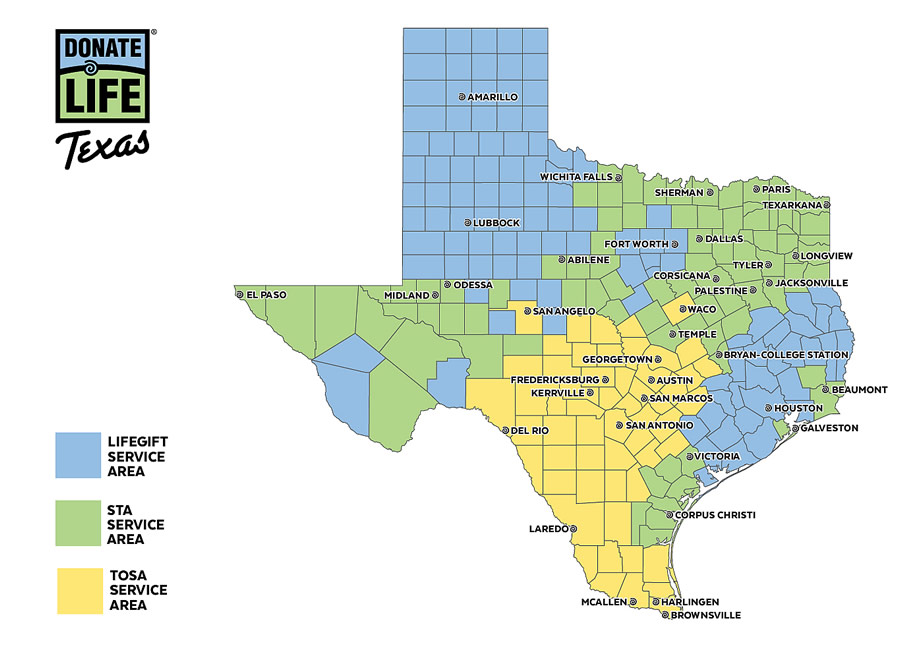
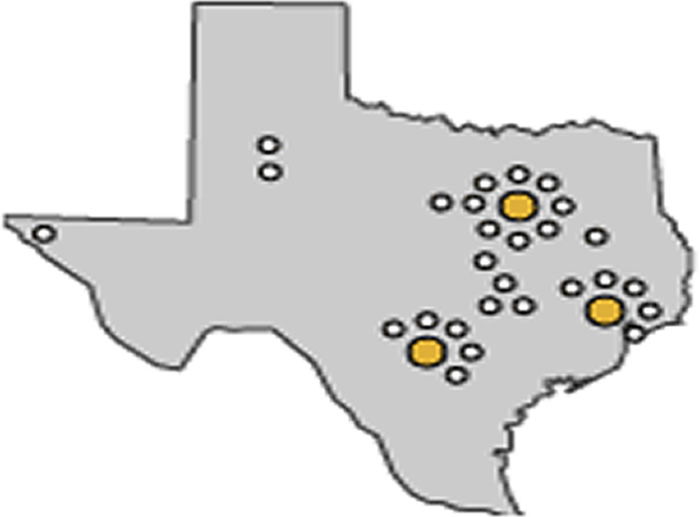
Figure 2. Active kidney transplant centers in Texas (white circles) and 3 organ procurement organizations home bases (yellow circles)