VOLUME 31, ISSUE 1

Adam C. Adler, MD, MS, FAAP, FASE
Department of Anesthesiology
Perioperative and Pain Medicine
Texas Children’s Hospital
Baylor College of Medicine
Houston, TX

Arvind Chandrakantan, MD, MBA, FAAP, FASA
Department of Anesthesiology
Perioperative and Pain Medicine
Texas Children’s Hospital
Baylor College of Medicine
Houston, TX
Taking the Hocus out of PoCUS: An Update on Point of Care Ultrasound
Overview of Point of Care Ultrasound
Point-of-care-ultrasound (PoCUS) has become mainstream in a host of acute care specialties owing to a growing list of applications (Table 1). However, despite its well documented use, adoption by anesthesiologists remains lagging with concerns related to lack of training, fear of missing diagnoses, and a lack of a certification pathway[1, 2]. While most of the PoCUS utilization and research has been centered around other acute care specialties (critical care, emergency medicine), there is growing evidence to dispel these concerns provided proper training and oversight. This speaks to the tremendous amount that PoCUS can add to anesthesiology practice.
Point-of-care-ultrasound has emerged as an invaluable tool for real-time physical examination assisted diagnosis with numerous studies highlighting improved accuracy over traditional physical examination[3]. PoCUS requires learning to identify a series of ultrasonographic signs indicative of pathology, particularly related to the cardiopulmonary system[4]. Using a few selected ultrasonographic views, anesthesiologists can attain a vast amount of qualitative clinically relevant information (table 2). At present, PoCUS should be applied to address a specific clinical question. It is possible that the future of perioperative medicine will consist of a brief pre-operative scan in addition to, or perhaps in lieu of, traditional palpation/auscultation.
In the perioperative period, PoCUS can provide a wealth of real-time information helping to guide patient management[5]. Envision the ‘on-call’ scenario in which an 86-year-old female arrives for a repair of hip fracture after an unwitnessed fall. She is confused and hypovolemic and a loud murmur is auscultated at the right sternal boarder. In this situation PoCUS may help the anesthesiologist understand the source of the murmur (i.e. severe/critical aortic stenosis vs. mild), the basic overall ventricular function and the general degree of hypovolemia (figure 1). Practically speaking, should the case be delayed for medical optimization, further cardiac evaluation, or to await the presence of a cardiac trained anesthesiologist. Additionally, PoCUS may help guide fluid resuscitation in the pre-operative area prior to proceeding with surgery. It is situations like this where a brief and easily obtainable bedside PoCUS evaluation can aid the anesthesia anesthesiologist’s management decisions.
Numerous studies have highlighted the successful implementation of PoCUS in perioperative management. Canty et. al. report a 54% change in anesthetic management when bedside ultrasound was used as part of the preoperative evaluation in patients with symptoms of cardiac disease or those believed to be at high risk for cardiac disease[6]. Similarly, Cowie et. al. demonstrated a high incident of change of management when PoCUS was used to assess a variety of perioperative issues[7]. PoCUS may be used to augment and enhance traditional physical examination and can be extremely valuable in all perioperative phases.
How can I learn Point of Care Ultrasound?
While not difficult, learning PoCUS and being able to successfully demonstrate proficiency to incorporate its use into clinical practice requires some individual effort. To acquire the skills necessary to perform PoCUS in the clinical setting, providers must demonstrate proficiency in image acquisition and interpretation as determined by local oversight committees for quality assurance[5] (figure 2). Proficiency in image acquisition may be improved through attendance at an ultrasound course available through a number of medical societies. Hands on didactic seminars are available at most Anesthesiology and Critical Care national meetings including: The American Society of Anesthesiologists, Society for Pediatric Anesthesia, Society of Cardiovascular Anesthesiology and Society of Critical Care Medicine. While there is no definitive number of scans noted to demonstrate proficiency, a number of studies have suggested that roughly 10-12 hours of training and around 25 performed PoCUS examinations are required to establish reasonable proficiency[8, 9].
Image interpretation and, specifically, the ability to discern pathology from normal anatomy requires self-teaching by review of the numerous ultrasound materials available on a host of websites such as the American College of Cardiology website on PoCUS (https://www.acc.org/latest-in-cardiology/articles/2017/10/31/09/57/point-of-care-ultrasound). See et. al. demonstrated that with self-guided reviewed of ultrasound images, correlation with expert findings for basic pathologies may be achieved after 30 examinations for a novice sonographer[10].
While still not mainstream, a number of organizations are offering PoCUS certification (e.g. The American College of Chest Physicians). However, starting in 2019, certification in critical care echocardiography will be offered by the National Board of Echocardiography. Certification will demonstrate quality assurance to providers wishing to augment their practice with PoCUS.
Ensuring Safe Use of Point of Care Ultrasound in My Practice
As with any new technology local expert oversight is recommended to ensure basic competency and skills. At Texas Children’s Hospital, we developed a PoCUS collaborative with pediatric stakeholders from the neonatal and pediatric intensive care units, emergency medicine, anesthesiology, adolescent gynecology, cardiology, and radiology. The goal of this collaborative is to provide oversight for the application of technique, knowledge, and certification/credentialing (i.e. quality control) to assure high quality cross-disciplinary PoCUS practices. With the ever-expanding utility of point-of-care ultrasound being recognized across subspecialties, anesthesiologists are urged to consider how this (21st century stethoscope) may be utilized in our dynamic perioperative environment.
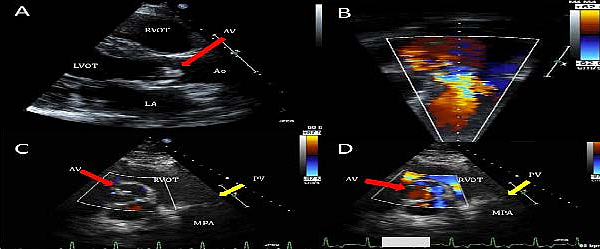
Figure 1: Identification of severe aortic stenosis by point-of-care ultrasound. The goal of PoCUS in this example is for the provider to recognize a small aortic valve opening with severe flow restriction. This can assist with perioperative planning. Reproduced with permissions from Adler AC, et. al. J Cardiothorac Vasc Anesth 2016;30(2):521-9[5].
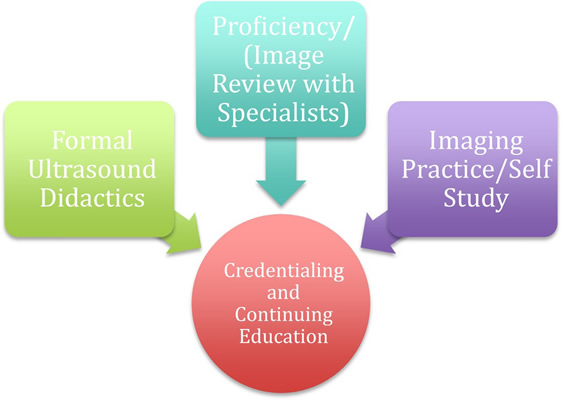
Figure 2: Suggested pathway for acquiring the skills and knowledge to perform PoCUS in clinical practice. Reproduced with permissions from Adler AC, et. al. J Cardiothorac Vasc Anesth 2016;30(2):521-9[5].
Table 1: Common applications of Point of Care Ultrasound in Acute Care Practice
| System | Examples of PoCUS Applications |
|---|---|
| Abdominal | Volume status, free fluid |
| Airway Examination | Endotracheal tube placement/cricoid membrane location |
| Cardiac Arrest | Reversible causes of arrest, presence of intrinsic activity |
| Cardiac examination | Pericardial effusion, ventricular, and valvular function |
| Gastric | Gastric volume/contents |
| Genitourinary | Bladder volume, scrotal ultrasound |
| Hemodynamics & resuscitation | Volume status and response to fluid boluses |
| Soft tissue examination | Abscess, foreign bodies |
| Ocular examination | Intracranial pressure, optic nerve swelling |
| Physical examination assistance | Murmur differentiation, volume status, cardiac function |
| Pulmonary examination | Pleural effusions, pneumothoraces, pneumonias, atelectasis |
| Regional Blocks | Nerve blocks |
| Trauma | FAST scan, pneumothoraces |
| Vascular Access | Intravenous and arterial line placements |
Table 2: Common pathologies identified in basic PoCUS applications.
Reproduced with permissions from Adler AC, et. al. J Cardiothorac Vasc Anesth 2016;30(2):521-9[5].
References

References
- Conlin F, Connelly NR, Raghunathan K, Friderici J, Schwabauer A: Focused Transthoracic Cardiac Ultrasound: A Survey of Training Practices. Journal of cardiothoracic and vascular anesthesia 2015. J Cardiothorac Vasc Anesth. 2013; 27(5):955-7.
- Conlin F CN, Eaton MP, Broderick P, Friderici J, Adler AC. : Perioperative Use of Focused Transthoracic Cardiac Ultrasound: A Survey of Current Practice and Opinion. Accepted for publication Anesthesia and Analgesia. Anes analg. 2017; 125(6):1878-1882.
- Spencer KT, Anderson AS, Bhargava A, Bales AC, Sorrentino M, Furlong K, Lang RM: Physician-performed point-of-care echocardiography using a laptop platform compared with physical examination in the cardiovascular patient. J Am Coll Cardiol. 2001; 15;37(8):2013-8.
- Spencer KT, Kimura BJ, Korcarz CE, Pellikka PA, Rahko PS, Siegel RJ: Focused cardiac ultrasound: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2013 Jun;26(6):567-81.
- Adler AC, Greeley WJ, Conlin F, Feldman JM: Perioperative Anesthesiology UltraSonographic Evaluation (PAUSE): A Guided Approach to Perioperative Bedside Ultrasound. J Cardiothorac Vasc Anesth. 2016; 30(2):521-9.
- Canty DJ, Royse CF, Kilpatrick D, Bowman L, Royse AG: The impact of focused transthoracic echocardiography in the pre-operative clinic. Anaesthesia 2012, 67(6):618-625.
- Cowie BS: Focused transthoracic echocardiography in the perioperative period. Anaesth Intensive Care. 2010; 38(5):823-36
- Manasia AR, Nagaraj HM, Kodali RB, Croft LB, Oropello JM, Kohli-Seth R, Leibowitz AB, DelGiudice R, Hufanda JF, Benjamin E et. al: Feasibility and potential clinical utility of goal-directed transthoracic echocardiography performed by noncardiologist intensivists using a small hand-carried device (SonoHeart) in critically ill patients. Journal of cardiothoracic and vascular anesthesia 2005, 19(2):155-159.
- Gaspar HA, Brunow de Carvalho W, Delgado AF: How to Train and Maintain Pediatric Intensivists Updated in Focused Cardiac Ultrasound? Pediatr Crit Care Med. 2016; 17(10):1015
- See KC, Ong V, Ng J, Tan RA, Phua J: Basic critical care echocardiography by pulmonary fellows: learning trajectory and prognostic impact using a minimally resourced training model*. Crit Care Med. 2014; 42(10):2169-77

