VOLUME 31, ISSUE 2

Emily Garmon, MD
Baylor Scott & White Temple Department of Anesthesiology
Clinical Assistant Professor
Texas A&M Health Science Center College of Medicine
Medical Director, Temple Acute Pain Management Service
Temple, TX

Shawn R. Schepel, MD
Baylor Scott & White – Memorial Department of Anesthesiology
Cardiothoracic Anesthesiology Fellow
Texas A&M Health Science Center College of Medicine
Temple, TX
Regional Anesthesia at the Serratus Plane
Thoracic trauma and surgery are frequently associated with moderate to severe pain. Poorly controlled acute pain is associated with detrimental physiologic consequences, multi-organ dysfunction, delayed recovery, and increased risk of developing chronic pain.1 Thoracic epidural or paravertebral catheters have traditionally been used to provide superior analgesia, improve pulmonary function, and reduce adverse effects associated with systemic opioid analgesia.2 However, epidural catheters are associated with increased risk of hypotension, urinary retention, pruritis, and motor weakness.3 Rarely, more serious complications occur, including epidural hematoma, epidural abscess, and persistent neurological injury.4 Although paravertebral techniques are associated with fewer adverse effects, catheter tip entry into the epidural space occurs in up to ten percent of paravertebral catheters placed with an anatomic approach, and the incidence of local anesthetic spread to the epidural space may be even higher when ultrasound guidance is used.5,6 Thus, lower risk peripheral techniques to treat thoracic wall pain have been proposed.7
The serratus plane block was first described by Blanco and colleagues for the treatment of unilateral chest wall pain associated with mastectomy.8 Further studies have demonstrated efficacy for the management of pain associated with thoracotomy and traumatic rib fractures, with fewer adverse effects than thoracic epidural analgesia.9,10,11 Benefits of the block include avoidance of risks associated with neuraxial catheter placement, ease of patient positioning, and potential for use in outpatient procedures. The serratus plane block targets the lateral cutaneous branches of the intercostal nerves that innervate the hemithorax and is performed at the level of the fifth rib. Spread of local anesthetic in the plane superficial or deep to the serratus anterior muscle reliably produces analgesia between the T2-T9 dermatomes, but spares the anterior cutaneous branches innervating the anterior chest wall and sternum, the posterior primary rami innervating the posterior wall and spine, and the supraclavicular nerves innervating the clavicle.8 It also spares the autonomic nerve fibers, which are responsible for hemodynamic variability with neuraxial and paravertebral techniques.
The block could theoretically be performed using an anatomic approach targeting the fifth rib, but ultrasound guidance provides visual confirmation of local anesthetic spread in the targeted tissue plane. The patient may be positioned either supine or lateral with the ipsilateral upper extremity abducted away from the body. Optimal imaging for most patients can be achieved with the wide linear ultrasound transducer positioned in the sagittal plane at the mid-axillary line overlying fifth rib. Muscular landmarks described by Blanco include the latissimus dorsi (superficial and posterior), teres major (superior), and serratus muscles (deep and inferior).8, The needle is advanced superior-to-inferior using an in-plane approach until just deep to the latissimus dorsi muscle and superficial to the serratus anterior muscle (superficial approach) or just deep to the serratus anterior muscle and superficial to the rib (deep approach). As with other tissue plane blocks, the suggested volume of local anesthetic for an effective block is 30-40 mL. Duration of blockade may be increased when the superficial approach is used.8 For prolonged blockade, catheter placement at the serratus plane has been described.10
The figures below depict sequential imaging of a deep approach to the serratus plane block in a thin woman with multiple rib fractures. The wide linear transducer was used, oriented cephalad to caudad. The depth shown is 3 cm. As discussed above, the muscular landmarks were identified prior to needle entry. The needle was advanced in-plane to the cephalad surface of the fifth rib. After negative aspiration, 10 mL of bupivacaine 0.25% was injected (Figure 1). Thereafter, the needle was advanced caudad over the fifth rib while the remaining 20 mL volume was injected The growing volume of literature demonstrating simplicity, analgesic efficacy, and safety of the serratus plane block for the treatment of unilateral chest wall pain warrants its consideration as a lower risk alternative to neuraxial or paravertebral techniques in certain patient populations.
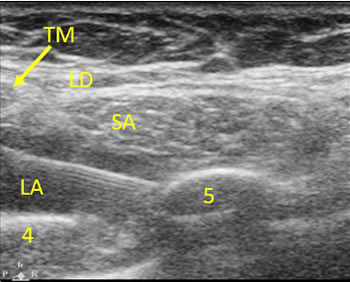
Figure 1. Transducer orientation is cephalad (left) to caudad (right). Depth is 3 cm. The arrow points to the border of the teres major muscle (TM), which is superior and deep to the latissimus dorsi muscle (LD). The serratus anterior muscle (SA) is inferior to the teres major muscle and deep to the latissimus dorsi muscle. The needle is clearly seen entering from the cephalad direction, with the tip at the cephalad surface of the fifth rib (5). Local anesthetic (LA) spread above the fourth rib (4) is visible after injection of the first 10 mL.

Figure 2. After injection of the first 10 mL local anesthetic (LA), the needle is advanced over the fifth rib (5), with continued injection of local anesthetic. Intercostal muscles (ICMs), pleura (P), and fifth rib (5) are clearly demonstrated deep to the local anesthetic spread. Teres major muscle is no longer visible, but latissimus dorsi (LD) and serratus anterior (SA) are indicated.
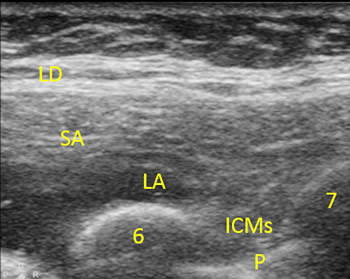
Figure 3. After injection of 30 mL local anesthetic and removal of the needle, local anesthetic (LA) is demonstrated overlying the sixth rib (6) and extending toward the seventh rib (7), deep to the latissimus dorsi (LD) and serratus anterior (SA) muscles and superficial to the intercostal muscles (ICMs) and pleura (P).
References
- Joshi GP, Ogunnaike BO. Consequences of inadequate postoperative pain relief and chronic persistent postoperative pain. Anesthesiology Clin N Am 2005; 23:21-36
- Ballantyne JC, Carr DB, deFerranti S, et al. The comparative effects of postoperative analgesic therapies on pulmonary outcome: cumulative meta-analysis of randomized, controlled trials. Anesth Analg 1998; 86:598-612
- Popping DM, Elia N, Van Aken HK, et al. Impact of epidural analgesia on mortality and morbidity after surgery: Systematic review and meta-analysis of randomized controlled trials. Ann Surg 2014; 259:1056–1067
- von Hosslin T, Imboden P, Luthi A, et al. Adverse events of postoperative thoracic epidural analgesia, a retrospective analysis of 7273 cases in a tertiary care teaching hospital. Eur J Anaesthesiol 2016; 34:1–7
- Luyet C, Siegenthaler A, Szucs-Farkas Z, et al. The location of paravertebral catheters placed using the landmark technique. Anaesthesia 2012; 67:1321–6
- Neal JM, Brul R, Horn JL, et al. The second American Society of Regional Anesthesia and Pain Medicine evidence-based medicine assessment of ultrasound-guided regional anesthesia executive summary. Reg Anesth Pain Med 2016; 41:181–94
- Rawal N. Epidural technique for postoperative pain gold standard no more? Reg Anesth Pain Med 2012; 37:310-17
- Blanco R, Parras T, McDonnell JG, et al. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia 2013; 68:1107-13
- Madabushi R, Tewari S, Gautam SK, et al. Serratus anterior plane block: a new analgesic technique for post-thoracotomy pain. Pain Physician 2015; 18:E421-E424
- Fu P, Weyker PD, Web CA. Case report of serratus plane catheter for pain management in a patient with multiple rib fractures and an inferior scapular fracture. A&A Case Reports 2017; 8:132–5
- Khalil AE, Abdallah NM, Bashandy GM, Kaddah TA. Ultrasound-guided serratus anterior plane block versus thoracic epidural analgesia for thoracotomy pain. J Cardiothorac Vasc Anesth 2017; 31:152-8
