VOLUME 35, ISSUE 2

William C. Culp, Jr., M.D.
Professor of Anesthesiology
Associate Dean of Faculty Affairs & Faculty Development
Vice Chair of Academic Affairs
Baylor College of Medicine- Temple
Baylor Scott & White Medical Center
Temple, TX
Adult Cardiothoracic Anesthesiology Fellowship Match Update
This year’s Adult Cardiothoracic Anesthesiology Fellowship match results mark the second year in a row in which a significant number of training positions went unfilled. Is this merely a temporary aberration, or does this represent a new trend in post-residency training? What might be the cause, and what are the implications for the future? Let’s examine the data and see what this might mean.
Nearly 50 years ago, the Society of Cardiovascular Anesthesiologists was created to support and advance the specialized practice of anesthesiology for patients undergoing cardiac surgery. As surgical candidates became sicker and procedures heightened in intensity, the technological challenges for anesthesiologists grew. This led to an increased demand for cardiac anesthesiologists. In 2006, the Accreditation Council for Graduate Medical Education approved the creation of a standardized fellowship. The subspecialty has continued to mature, now requiring cardiac anesthesiologists to have a deep cardiac knowledge base and be proficient in a wide array of technical procedures, including invasive hemodynamic monitoring, echocardiography, cardiopulmonary bypass, mechanical assist devices, extracorporeal membrane oxygenation and transplant, among others.
The expertise produced by fellowship training has recently been recognized by the American Board of Medical Specialties, which in 2021 agreed to approve formal board certification in Cardiac Anesthesiology.i This complements the Advanced Perioperative Transesophageal Echocardiography Board Certification by the National Board of Echocardiography, first offered in 1998. For many years now, almost all academic faculty cardiac positions have required fellowship training. Over the last decade, private practice positions providing cardiac anesthesia have increasingly required some demonstration of formal echocardiography certification (such as typically follows fellowship training) in order to be credentialed to perform TEE, although this is far from universal. It is common for cardiac cases in private practice to be performed by non-fellowship trained anesthesiologists. Many of these anesthesiologists have supplemented their skills with cardiac anesthesiology related to CME.
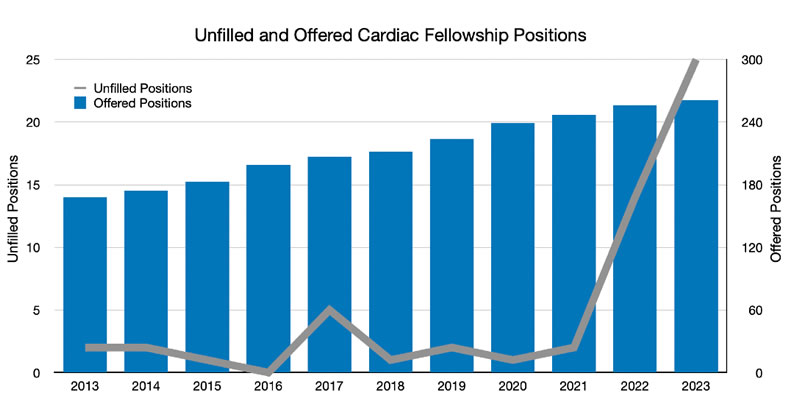
It is with this background that we can begin to interpret the cardiac fellowship match data over the last ten years. Cardiac fellowship positions increased from 168 positions in 2013 to 261 in 2023. Virtually all of these positions were filled each year, until 2022 and 2023 when there were 14 and 25 positions left unfilled, respectively.
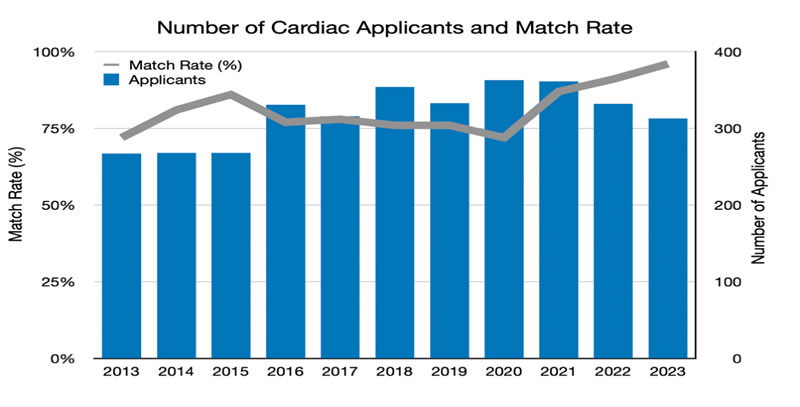
The match rate since 2013 ranged from 72%-87% until the last two years, with 96% of positions filled with the most recent match. These data reflect that cardiac fellowships have remained quite competitive even with expanding numbers of positions, mirroring the increased job demand for cardiac fellowship trained anesthesiologists- except for the last two years when nearly all applicants matched, and some positions went unfilled.ii
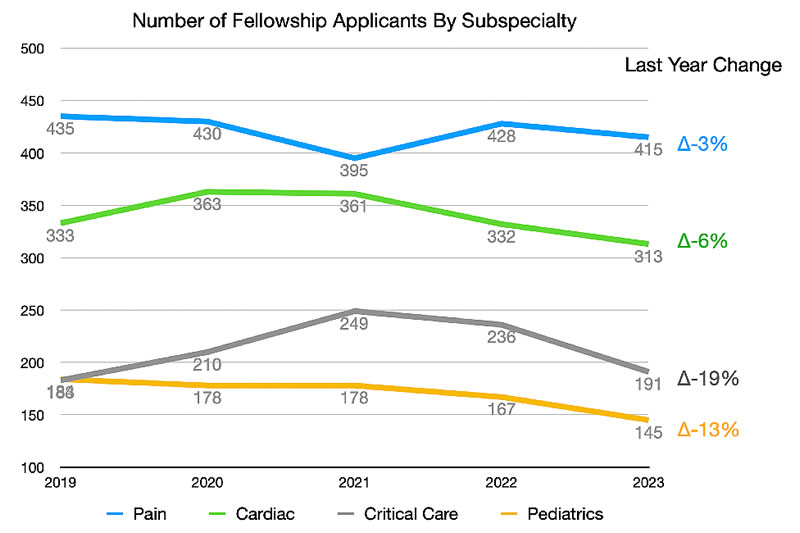
Why has the number of applicants decreased? Is this due to fewer graduating anesthesiology residents or a decreased interest in cardiac anesthesiology specifically? Thirty years ago, the advent of a then-new medical care delivery model, the Health Maintenance Organization, was projected to dramatically decrease national surgical volume and reflexively led to a precipitous drop in anesthesiology residents seemingly overnight. Only 17% of residency positions were filled with graduating American medical students at the nadir in 1996. Our specialty has since recovered with 99.8% of positions matched in 2023, providing strong evidence that the field remains popular and competitive. In contrast, interest in fellowships is decreasing, with drops in applicants ranging from 3% in pain to 19% in critical care last year.iii
If the graduating resident supply remains strong, the largest driving factor for the decrease in cardiac fellowship interest is likely market forces similarly impacting other anesthesiology fellowships. Cardiac anesthesiologist positions remain in demand; however, general anesthesiology positions are in very high demand. The national labor shortage post-COVID is a huge challenge across many industries, including health care in general and anesthesiology in particular. These shortages are driving high starting salaries and signing bonuses. Private practices are more willing to accept non-fellowship trained anesthesiologists who have a cardiac specialty interest with the expectation of on-the-job training and CME to meet expected performance during cardiac cases. The cost of a fellowship is significant, and with student debts of $250,000 or more coupled with inflation, the return-on-investment calculation may not favor additional training for some. Further, there is mixed messaging from anesthesiology societies that may encourage or discourage fellowship training, depending on context.
So, what should we do about cardiac and our other fellowship training programs? Certainly, close attention to match data in the next few years is warranted. Market cycles can move quickly and attention to data may allow programs to react in a timely manner to enhance recruiting efforts. At the same time, we should appreciate that this trend is not unique to anesthesiology, with other specialties struggling due to market forces.iv Expansion of fellowship training programs or creating new programs is likely inappropriate at this time unless other program closures result in no net growth. We should ensure that residents are not only exposed to our subspecialties, but also shown the benefits of fellowship training in order to make informed decisions to best meet their individual financial and professional career goals. The need for fellowship trained cardiac anesthesiologists will continue, particularly in academic practices and large hospital centers, and it remains our job- and our privilege- to help train those who want to invest in developing these skillsets.
Sources:
Troianos CA, Shaw AD. Cardiac anesthesiology subspecialty certification: a step forward in cardiac perioperative medicine. ASA Monitor, December 2021, Vol. 85, 39.
SFMatch Residency and Fellowship Match Services. www.sfmatch.org last accessed June 2023
The Match: National Resident Matching Program. www.nrmp.org last accessed June 2023
Simons, SS. Grads know that EDs are dumpster fires. Emergency Medicine News June 2023, 45(6): 1,29.
